
Dyspareunia (pain during intercourse) - Symptoms, Causes & Treatment
Almost a third of young girls and half of adult women have experienced pain or discomfort during intercourse, caused, in most cases, by inflammation present in the vagina or labia.
If you feel pain during or after sex, your body may be trying to tell you that something is wrong, so don't ignore it. It's time to talk about dyspareunia.
Is pain during intercourse normal?
Many women feel a degree of discomfort or pain during intercourse. If the intensity is not so great that it affects the quality of sexual life or leads to the interruption of sexual contact, or if the pain is only occasional and is not accompanied by other symptoms, then there is no need to worry. If, on the other hand, the pain is strong, repetitive, accompanied by other symptoms, then it is time to contact the gynecologist. 
The medical term for painful intercourse in women is dyspareunia, defined as persistent or recurring genital pain that occurs right before, during, or after sex. It is a common condition that can have negative emotional and psychological effects. In addition to physical pain, we can suffer from the loss of intimacy or it can be a cause of stress in the relationship with the partner.
Fortunately, the causes of this condition can be treated.
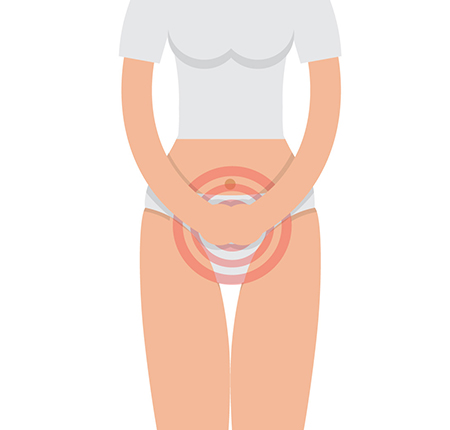
Dyspareunia - Symptoms
There are two types of dyspareunia:
- superficial, when the pain is felt at the entrance to the vagina or inside the vagina (affecting the vulva and opening of the vagina);
- deep (or abdominal), when the woman feels the pain in the abdomen.
If you have painful intercourse, you may experience:
Pain only during intercourse (penetration)
Pain with every penetration, including inserting a tampon
Deep pain during pushing
Burning pain or soreness
Throbbing pain that lasts for hours after intercourse
Burning sensation
Vaginal dryness
Vaginal bleeding during or immediately after intercourse
Pelvic cramps
Pain during intercourse - Causes
Pain during intercourse can have a physical cause or an emotional cause, and sometimes, they can even overlap. For example, a physical problem not resolved in time can create anxiety about intercourse, which makes it difficult to relax and leads to additional tension in the vaginal muscles.
Physical causes include:
Insufficient lubrication - can occur when foreplay is too short, during breastfeeding or menopause when the level of estrogen is low, when using drugs from the class of oral contraceptives, antidepressants, sedatives, antihypertensives or antihistamines.
Injury or trauma to the vagina - acquired as a result of an accident, surgical intervention in the pelvic area, episiotomy from childbirth.
Vaginal inflammation or infection - given by bacteria or fungi (mushrooms) that can lead to irritation of the vagina.
Vaginismus - represents the involuntary contraction of the muscles of the vagina, which causes the sensation of stinging and pain during attempts to have sexual contact, and unfortunately we have no control over the mechanism that triggers it.
Vulvodynia - is the pain in the vulva, caused by the weakness of the pelvic muscles, hypersensitivity to the vaginal flora, damage to the vulvar muscles due to the presence of a greater number of sensitive nerves innervating the vulvar area
Psychosexual problems can also interfere with intercourse, leading to pain:
trauma from sexual abuse
unpleasant initial sexual experiences
personality changes
depression
anxiety, feeling of shame, guilt
fear of a possible pregnancy
religious education
lack of adequate sex education
Superficial dyspareunia - Pain at initial penetration
Pain on initial penetration can be associated with a number of factors, including:
Not enough lubrication - This is often the result of insufficient foreplay. A drop in estrogen levels after menopause or childbirth or during breastfeeding can also be a cause.
Certain medications can affect sexual desire or arousal - They can reduce natural lubrication and sex can become painful. Such drugs include antidepressants, blood pressure medications, sedatives, antihistamines, and certain birth control pills.
Injury, trauma or irritation - These include injury or irritation from an accident, pelvic surgery, female circumcision or cuts made during childbirth to widen the birth canal (episiotomy).
Inflammation, infection or skin disorder - An infection in the genital area or urinary tract can cause painful intercourse. Eczema or other skin problems in the genital area can also be the problem.
Vaginismus - These involuntary spasms of the muscles of the vaginal wall can make penetration painful.
A problem present at birth - A vagina that is not fully formed (vaginal agenesis) or develops a membrane that blocks the vaginal opening (imperforate hymen) could cause dyspareunia.
Deep dyspareunia - Pain on deep penetration
Deep pain usually occurs on deep penetration. The pain may be more intense in certain sexual positions. Causes include:
Certain diseases and conditions.
The list includes endometriosis, pelvic inflammatory disease, uterine prolapse, retroverted uterus, uterine fibroids, cystitis, irritable bowel syndrome, pelvic floor dysfunction, adenomyosis, hemorrhoids, and ovarian cysts.
Surgical interventions or medical treatments.
Scarring from pelvic surgery, including hysterectomy, can make intercourse painful. Medical treatments for cancer, such as radiation and chemotherapy, can cause changes that make sex painful.
Emotional factors for pain during sex
Emotions deeply impact sexual activity, so they can play a role in sexual pain. Emotional factors include:
Psychological problems - Anxiety, depression, concerns about your physical appearance, fear of intimacy or relationship problems can contribute to low arousal and the resulting discomfort or pain.
Stress - Your pelvic floor muscles tend to tighten in response to stress in your life. This can contribute to pain during intercourse.
History of sexual abuse - Not everyone with dyspareunia has a history of sexual abuse, but if you have been abused, it can affect subsequent sexual intercourse.
Dyspareunia in men
Just like women, men can also feel pain if there is not enough vaginal lubrication during sex. This can be solved by using a sex lubricant. In men, painful sex can be caused by certain disorders of the penis:
Damage to the foreskin: Damage to the foreskin (the skin covering the head of the penis) caused by rubbing or tearing can lead to pain.
Sexually Transmitted Infections (STIs): Yeast infections or infections under the foreskin, as well as common STIs such as genital herpes or gonorrhea, can make sex painful.
Penile deformities: Peyronie's disease or other penile deformities can make intercourse painful.
Painful erections: A condition such as priapism can lead to persistent and painful erections.
Dyspareunia - When should you go to the doctor?
If you have recurring pain during sex, it's time to talk to your gynecologist. Treating the problem helps your sex life, emotional intimacy and self-image.

You should talk openly with your doctor about any pain during intercourse so that you can more easily identify the cause and choose the right treatment. Some questions your doctor may ask you are:
- When did the pain start?
- Where does the pain occur - describe the painful area as accurately as possible, at the entrance to the vagina or deep?
- Does the pain change with position?
- How intense is the pain on a scale of 0 to 10?
- How often does the pain occur?
- Does the pain pass spontaneously or are anti-inflammatories necessary?
- How long have you had painful intercourse?
- What medications are you taking?
- Have you had any surgery in the area?
- Have you been treated for any vaginal condition?
- Does the partner know about this problem? Does he want to help you?
- Are there other reasons that could be contributing to your pain? For example a stressful time or when you could be depressed?
How to make the correct diagnosis in case of dyspareunia?
The next step is the consultation on the gynecological table to evaluate possible signs of vaginal dryness, abnormal vaginal discharge, inflammation, anatomical problems, scars, lesions suggestive of endometriosis. During the examination, vaginal secretion samples and Pap tests can be collected.
Transvaginal ultrasound will indicate what is happening inside the pelvis, if there are ovarian cysts, fibroids, signs of inflammation or endometriosis. In rare cases where the ultrasound was not conclusive enough, an imaging investigation called a pelvic MRI may be indicated.
Also, psychological counseling may be necessary to determine possible emotional causes. This is to complete the diagnosis.
Dyspareunia - Treatment for vaginal pain
Sexual disorders are treatable. Treatment is different depending on the cause of the pain. The doctor can recommend various treatments depending on the cause of the pain, that's why the gynecological consultation and establishing the diagnosis is so important.
Drug treatment
Vaginal infection is perhaps the easiest to treat because we have many antibiotics and antifungals, both oral and intravaginal. In some cases, the partner must also receive treatment. And for pelvic inflammatory diseases, antibiotic treatment is also needed.
Surgical treatment
Pelvic pathologies such as endometriosis, ovarian cysts, fibroids or fallopian tube conditions often require surgery. The good news is that the intervention can be performed laparoscopically, therefore minimally invasive, with quick recovery and short hospitalization.
Vaginal exercises
It is good to know that there are techniques and exercises that can help reduce pelvic tension. Muscle treatment consists of:
stretching exercises at the levator anal muscle level
electrostimulation techniques with biofeedback
the kegel exercises we talked about in detail right here - perhaps the most effective way to strengthen your pelvic muscles, these exercises also help you get through the pain more easily.
Psychological counseling
In the absence of identifying a physical cause, cognitive-behavioral psychotherapy, couple therapy, relaxation techniques or to reduce anxiety are recommended. All these therapies can teach you how to restore your intimate life and improve communication with your partner.
Are there useful natural treatments for dyspareunia?
Before applying any treatment, it is best to consult a gynecologist. If you make a decision on your own, there is a risk that the problems will get worse. However, we have some suggestions that may be of use to you.
Use a water-based or silicone lubricant to help with vaginal dryness.
Try sexual activities or positions that don't cause you pain.
Try taking over-the-counter pain relievers before sex.
Take time to relax before having sex.
Apply ice packs to the vulva after intercourse.
Stop using vaginal perfumes, bubble baths or scented tampons.
Frequently asked questions
If we haven't answered your questions yet, here are some frequently asked questions and the answer you needed.
Can dyspareunia cause vaginal bleeding?
Dyspareunia does not necessarily cause bleeding. Any bleeding that occurs during intercourse is likely caused by the underlying medical problem. Bleeding could be caused by the same problem that causes painful sex.
And as the first step to health is the decisions you make, absorbents and organic tampons , such as ENROUSH made from 100% organic cotton , take care of you and do not pose a risk to the planet. You prevent irritation and possible allergies and feel safe all day.

How long does recovery take after the disappearance?
Recovery time for dyspareunia varies depending on the underlying cause of the pain you feel during intercourse. The good news is that recovery from painful sex is possible. Whether it's medication, counseling, surgery, or the use of lubricant, your gynecologist can find a treatment that will help.
Can pain during sex be prevented?
There's usually not much you can do to reduce the risk of failure, it's often something we have no control over. However, you can choose to have safe, protected sex and maintain good hygiene.






















