
You've probably heard us talk about vulvovaginal health many times, and maybe you've heard the term vaginitis or vulvovaginitis before, but no one told you exactly what it means, how it affects you, and how to protect yourself from it. So today we talk extensively about this condition: what it is, when it occurs, how many types it is, how does vulvovaginitis manifest itself and what do we do to protect our intimate health? Let's take them one at a time.
What is vaginitis (vulvovaginitis)?
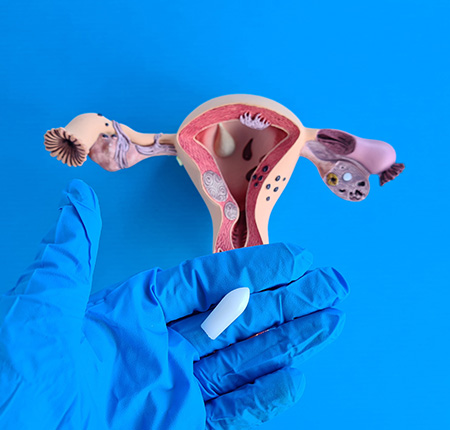
Vaginitis, also known as vulvovaginitis, is actually a broad medical term that defines infection or inflammation of the vulva or vagina (vulvovaginal area) due to various conditions. Like any inflammation, vaginitis is unpleasant and creates discomfort. Sensations of itching, burning, pain and unusual discharge appear.
However, the condition itself is not at all uncommon - it can occur at any age, and one in three women will experience at least one form of vaginitis in their lifetime. So you don't have to panic, just go to the gynecologist as soon as possible. Let's talk about how you get vulvovaginitis, how it manifests, and how we treat it.
Types of vulvovaginitis:
There are a lot of factors that can infect or inflame a woman's vagina and vulva—and depending on them, there are just as many types of vulvovaginitis.
The infection can be caused by a virus, bacteria or fungi. Inflammation can also occur in response to skin contact with allergens and harmful chemicals in care products such as shower gel or menstrual products. Including vaginal dryness, low estrogen or unprotected sex can lead to vulvovaginitis.
We will take these factors in turn to see what types vulvovaginitis falls into.

Bacterial vaginitis
It is the form of vaginitis that most commonly affects women who have not yet reached menopause. As you can guess from the name, it is caused by several bacteria. These bacteria are already normally in your vagina, but they end up causing vaginal inflammation when they overgrow, just like candida does when the vaginal pH is disturbed.
It is not a sexually transmitted disease, but it occurs more often in women with an active sexual life, and the main risk factors are changing sexual partners, vaginal douching and smoking.
It is important that bacterial vaginitis is correctly diagnosed. Don't confuse it with candidiasis and don't self-medicate, because the treatment for candida infections is different from that for bacterial infections and can make them worse!
Atrophic vaginitis
At the opposite pole of bacterial vaginitis, which occurs mainly before the menopause, atrophic vaginitis affects women especially in menopause and perimenopause, or after surgical removal of the ovaries. It is a form of non-infectious vaginitis that occurs as a result of low estrogen levels, when the vagina becomes dry.
The vagina can also become drier and atrophic during breastfeeding and postpartum periods, so you are prone to atrophic vaginitis if you are in this category as well. Also, treatment for endometriosis or breast cancer can lead to a low level of estrogen, thus increasing the risk of atrophic vaginitis.
Acute vaginitis
This time from the point of view of the stage of the condition - and not the causes - we can classify it into:
acute vaginitis, which we are talking about now;
chronic vaginitis - about which we will talk a little below.
The acute form is the most common, and is what we mean when we talk about bacterial and candidal vulvovaginitis. The acute symptoms of vulvovaginitis also refer to inflammation of the vulva due to sexually transmitted infections, such as trichomoniasis, Chlamydia or Gonorrhea.
It is manifested by burning sensations, pain, itching, vaginal discharge and pain during sexual intercourse.
Mycotic / fungal vaginitis (candidiasis)
Fungal (mycotic) infections are the second most common cause of inflammation of the vulva and vagina. The most common cause of fungal vaginitis is infection with Candida albicans or other candida species.
Candidiasis occurs, as we said above, when something disturbs your vaginal balance, and candida proliferates excessively. This can happen including:
if you are pregnant and hormonal changes occur;
if you have diabetes and the level of glucose in your urine and vagina is too high;
after taking antibiotics, which also kill the good bacteria normally found in the vagina.
But did you know that I talked about candidiasis on the blog in a previous article? You can read it HERE to learn more about preventing and treating Candida albicans infection.
Non-infectious vaginitis
Vulvitis (ie inflammation of the vulva) or vaginitis can also occur without an infection. In this case, we are talking about non-infectious vulvovaginitis, which is simply an allergic reaction. It means that something is irritating your genital area without causing an infection.
The balance of the vaginal flora is delicate, and such irritations can occur both from products you use in the vagina, and from materials or substances that simply come into contact with the sensitive skin of your intimate area:
Spermicides;
Vaginal douches;
vaginal sprays;
Seminal fluid;
Foods you are allergic to (peanuts, chocolate, soy, eggs, nuts, etc.)
Feminine hygiene products containing perfumes and other harmful substances (soaps, shower gels, wet wipes, lubricants, creams);
Detergents and conditioners used for washing underwear;
Underwear made of synthetic materials that do not allow the skin to breathe;
Conventional menstrual products that contain plastic, dioxin, fragrances and other toxic ingredients.
Nonspecific vaginitis
Another way we can classify vaginitis into two types according to its origin is in:
Specific vaginitis, when it originates from specific agents such as viruses, fungi, bacteria, protozoa or arthropods. This category includes vaginitis caused by HPV (human papillomavirus), genital syphilis (Treponema pallidum bacteria) or trichomoniasis (Trichomonas vaginalis).
Nonspecific vaginitis, which occurs when the vaginal flora is out of balance.
There are several ways in which you can choose to have non-specific vaginitis, but they all boil down to the multiplication of bacteria that normally live in the vagina. Thus, factors that trigger the overgrowth of these bacteria include:
at the local level: the postpartum period or after an abortion, lack of proper hygiene in the intimate area, injuries after sexual intercourse;
in general: hormonal changes, diabetes, weakening of the immune system.
Trichomoniasis
Vulvovaginitis can also be triggered by sexually transmitted viruses, bacteria or parasites, and trichomoniasis is one such example. So are Gonorrhea and Chlamydia, the three most common causes of viral (sexually transmitted) vaginitis.
Foul-smelling vaginal discharge and itching are the most common signs of trichomoniasis, when the protozoan Trichomonas vaginalis (a small, single-celled parasite) infects your vagina. Men who transmit this parasite usually have no symptoms. It takes at least 7 days of sexual abstinence and that all partners follow the treatment to effectively get rid of such an infection.
Mixed vaginitis
You can understand from the name what mixed vaginitis refers to. It is very rare, and requires the existence of not one, but at least two infections (or two harmful agents) that simultaneously cause inflammation of the vulvovaginal area:
Bacterial vaginitis;
Herpes simplex;
Trichomonas vaginalis;
Neisseria gonorrhea;
Chlamydia trachomatis.
For example, we are talking about mixed vaginitis in a patient with trichomoniasis & other bacterial infection, candidiasis & other bacterial infection, or Chlamydia infection & other bacterial infection. In these cases, treatment for both conditions will need to be followed.
Chronic vaginitis
Much rarer than the acute vaginitis we told you about above, chronic - or persistent - vaginitis has the same symptoms as the acute form, only it lasts 6 months or even longer. The main reason is either that the symptoms appear and disappear after a period of time, or because the patient intuitively treats herself with creams or antifungals, without a visit to the gynecologist.
Once diagnosed and treated correctly, chronic vaginitis heals in a short time. The most common forms of chronic vaginitis are:
Inflammatory desquamative vaginitis (aerobic): which is manifested by irritation and inflammation of the genital area, purulent vaginal secretions and a strong feeling of discomfort.
Untreated atrophic vaginitis, which we have already discussed above that occurs especially during menopause;
Irritations, allergies and untreated dermatological problems in the intimate area.
Vaginitis - Symptoms:
The symptoms of vaginitis differ depending on the type of condition that each patient suffers from. You've already seen how many forms and causes vulvovaginitis has, and it's normal for the symptoms to be just as numerous and varied. But mainly, they all boil down to inflammation of the vulva and vagina, the most common symptoms being:
Unusual vaginal discharge;
Stinging sensation, itching, redness, burning;
Swollen organs in the genital area and inflamed vagina;
Burning, stinging or pain when urinating;
Pain and discomfort during intercourse and more. Pain during sexual intercourse is not, however, an exclusive symptom of vaginitis, but can have a lot of other causes, which we also talked about on our blog: Why do you feel pain during sex?
I have listed only some general signs and symptoms above. But depending on the type of vaginitis, they become specific, so let's see how the categories of vulvovaginitis mentioned above manifest. Here are the main symptoms of:
Bacterial vaginitis: inflammation of the labia and vulva, abnormal smell and milky, thin texture of the vaginal discharge, which becomes more unpleasant after menstruation or after intercourse; bacterial vaginitis can also be asymptomatic, in which case the doctor detects it only during a routine gynecological check-up.
Fungal/candidal vaginitis: vaginal redness and itching, thick and white or watery and odorless vaginal discharge, small sores on the vulva, burning sensation when urinating, and sometimes swollen vagina and sore labia.
Noninfectious vulvovaginitis: Swollen vulva, inflamed labia minora, burning and itching of the vulva and vagina, and thick, gelatinous, yellow or greenish vaginal discharge can be symptoms of allergic reactions without an infection.
Trichomoniasis: greenish-yellow color and unpleasant smell of vaginal secretions, pain and itching in the vulva and vagina, burning sensation when urinating and vaginal pain or discomfort in the lower abdomen during intercourse, which intensifies after menstruation. And inflamed labia are a symptom of trichomoniasis and genital syphilis.
Chlamydia: pain in the lower abdomen and pelvic area and light bleeding, especially after intercourse. Sometimes there is also vaginal discharge, but most of the time the symptoms are easy to overlook.
Herpes: small sores and lesions inside the vagina or in the vulva area, which can only be seen during a gynecological consultation. Pain caused by these lesions is the main symptom of herpes vaginitis.
HPV virus: White, gray, pink or purple genital warts may be present, but they do not always appear. Without visible signs, the human papillomavirus is detected only during a Pap test.
Vaginitis - Causes & risk factors:
We have already mentioned some of the main causes of vaginitis above, but now we will determine exactly what the causes and risk factors for vulvovaginitis are. So, let's start with the causes:
Bacterial, fungal, and viral infections are the causes of bacterial vaginitis, fungal vaginitis, and vaginitis caused by infection with viruses, bacteria, parasites, and other sexually transmitted agents, respectively.
The decrease in estrogen levels during menopause, perimenopause, after surgical removal of the ovaries or other hormonal problems are the causes of atrophic vaginitis.
Failure to treat acute vaginitis is the cause of chronic vaginitis;
Vaginitis caused by two or more simultaneous infections is the cause of mixed vaginitis;
Other causes of vulvovaginitis, or inflammation of the vulva and/or vagina, include:
Parasites: pinworms, scabies or lice in the intimate area;
Improper hygiene in the genital area;
Other sexually transmitted diseases;
The occurrence of a hormonal imbalance, for example after a birth or after an abortion;
Unbalancing the vaginal flora by using products with toxic ingredients for hygiene or intimate care.
And, last but not least, other risk factors that predispose patients to vaginitis are:
Starting sexual life with a new partner or frequently changing partners;
Using underwear and clothes made of synthetic materials, which do not allow the skin to breathe;
Using conventional menstrual products and feminine hygiene products that contain perfumes, bleaches, plastic, parabens or other harmful chemicals;
Food allergies;
Vaginal douches;
Treatments with antibiotics;
Failure to treat diabetes;
Problems with the thyroid or the endocrine system;
Estrogen-rich contraceptives;
Task;
Weakening of the immune system;
Smoking.
Vulvovaginitis during the summer
Some specialists say that the number of patients with vulvovaginitis increases by 50% during the summer, because the high level of humidity in the air and the increased temperature create the perfect environment for the imbalance of the vaginal flora and inflammation of the genital area.
To reduce this risk during periods of excessive heat, it is good to pay attention to clothes and hygiene habits, because they are the main risk factors. So avoid, as much as possible:
Synthetic clothes, thick and tight on the body: the skin needs to breathe, and synthetic fibers in underwear or pants retain sweat and moisture, favoring the disturbance of vaginal balance and the appearance of vaginitis. Organic cotton underwear and cool, airy clothes made of natural fibers are much more suitable both to prevent such ailments and for your comfort during the summer;
Wet clothes: again, sweating and maintaining moisture in the intimate area favors the multiplication of bacteria and the appearance of vaginitis. The intimate area must remain dry, and it is a good idea to use organic sanitary pads even on non-menstrual days, which absorb vaginal secretions and prevent the accumulation of moisture. If you exercise and sweat in the summer, take a shower and change into your workout clothes right after you finish;
Vaginal douches: unless your doctor recommends them, you do NOT need them! Your vagina has a slightly acidic pH naturally just to clean itself. Douching will throw your pH out of balance, so use only water and a natural intimate gel to clean only your vulva and the outside of your vagina.
Perfumed hygiene products: and perfumes in soaps, shower gels, sprays, intimate deodorants or absorbents, can disturb your pH balance. You don't need them - just use natural products without fragrance and other chemicals that are toxic to your skin.
Is vulvovaginitis transmitted?
Vulvovaginitis itself is not contagious, but the viral infections that cause it can be passed on to your partner. Trichomoniasis, Chlamydia, Gonorrhea, HPV, herpes - all these sexually transmitted diseases can be transmitted to a partner and can lead to vaginitis.
Also, bacterial vulvovaginitis is not transmitted, but unprotected sex with multiple partners can increase the risk of it occurring.
When should you consult a doctor?
It is always good to consult a doctor when you notice any kind of change in the color, smell or texture of your vaginal discharge, or if you experience discomfort and pain. Whether it's vulvovaginitis or another condition of the intimate area, diagnosis and treatment as soon as possible will help you get rid of symptoms more quickly and effectively.

It is all the more urgent to see a doctor if you suspect you have vulvovaginitis and notice the following signs:
You have foul-smelling vaginal discharge;
Vaginal secretions with unusual texture or yellow-green color appear;
You feel itching, burning, redness;
You notice the swelling of the genital area;
You have a stinging, burning or pain sensation when you urinate or during sexual intercourse;
You have never had a vaginal infection before;
You have recently had one or more new sexual partners;
You have a fever, pelvic pain or chills;
The symptoms of candidiasis do not disappear even though you have followed the prescribed treatment;
You have recently undergone antibiotic treatment.
Diagnosis of vulvovaginitis
To diagnose the cause and type of vulvovaginitis, the doctor may ask you questions about your medical history and perform a gynecological consultation. He will collect a sample to look at your vaginal secretions under a microscope, thus determining what caused your vaginitis.
They may also analyze your pH level to make a proper diagnosis. You may also be instructed to avoid sexual contact 24 hours before the consultation.
You can help your doctor make a correct diagnosis by describing all the symptoms you have noticed, namely any abnormal changes in vaginal secretions, the appearance of unusual odors in the intimate area or discomfort.
Treatment of vaginitis / vulvovaginitis:
The first step in the treatment of vulvovaginitis is the correct diagnosis, because the wrong treatment for the patient's type of vaginitis can make symptoms worse. Depending on the causes of the condition, the appropriate treatment will be chosen later.
For example, in non-infectious vaginitis, treatment is simply to stop using the products that may have caused the inflammation. This may mean replacing your shower gel or soap with a pH-neutral one, stopping using perfumed feminine hygiene products, opting for cotton underwear or changing your laundry detergent.
For the other types of vaginitis, the treatment may consist of the administration of special drugs or creams, which we will talk about next.
Drug treatment
Antibiotics are the main treatment for bacterial vulvovaginitis. As with trichomoniasis, the single-dose antibiotic is the treatment that both you and your partner must follow.
The same applies to the treatment of any other form of vaginitis caused by a sexually transmitted disease: both partners must be treated to prevent the spread and re-infection of the respective virus or parasite.
If vaginitis occurs as an allergic reaction, it is possible that in addition to removing the source that caused the irritation, the doctor will also recommend antihistamine drugs to relieve the symptoms.
Eggs for vulvovaginitis
In the case of mycotic vaginitis, ovules (vaginal suppositories) can be prescribed and inserted into the vagina to treat infections with various types of microorganisms. These eggs contain antifungal, disinfectant, anti-inflammatory and soothing ingredients that fight the infection and prevent its spread.
It is good to know that ova for fungal or candidal vulvovaginitis are oil-based, which is why they can reduce the effectiveness of latex condoms. For this reason, it is recommended to avoid sexual contact during treatment to avoid an unwanted pregnancy.
Creams for vulvovaginitis
Fungal infections can also be treated with antifungal creams or gels, and in the case of bacterial infections, an antibacterial cream can be prescribed. The doctor can also recommend an estrogen-based cream to treat atrophic vulvovaginitis, when the cause is hormonal changes.
Is vulvovaginitis natural treatment recommended?
Delaying or not treating vulvovaginitis at all is never recommended. Do not wait for the symptoms to go away on their own, as they may get worse. Also, naturopathic treatment is not recommended, except after a gynecological consultation and with the doctor's consent.

After a visit to the gynecologist and a correct diagnosis, if the doctor says it's okay, then you can also opt for a natural treatment at home, such as:
Baths with natural essential oils, without fragrance or dyes, which can hydrate the skin and reduce itching, redness, burning and stinging;
Sitz baths with a little vinegar, sea salt or tea tree oil to kill certain bacteria;
Topical antibacterial applications with coconut oil, crushed garlic, or a paste of water and baking soda;
Cold compresses to soothe inflammation and discomfort;
Warm baths with baking soda to relieve itching;
Consumption of probiotics There are several studies that claim that the symptoms of vaginitis can be improved by limiting the consumption of sugar and increasing the consumption of yogurt and probiotics containing lactobacilli.
Complications of vaginitis:
Without a correct diagnosis and proper treatment for the infections that caused the vaginitis, they can get worse. Untreated bacterial vaginitis and trichomoniasis can also lead to serious complications, including:
Problems in pregnancy: premature birth;
Pelvic inflammatory disease (PID);
Worsening of HIV infection or other sexually transmitted diseases.
Prevention of vaginitis
Preventing vaginitis actually means preventing the inflammations that occur when our vaginal flora is out of balance. That is, to prevent such imbalances, which we do by taking care of everything that comes into contact with our intimate area. Specifically, look how you can protect yourself as best as possible from infections and irritations that can cause vaginitis:
Keep your private area dry;
Avoid sitting in a wet bathing suit or sweaty workout clothes;
Also avoid synthetic, thick, body-hugging clothes, in which you sweat and retain moisture;
Wear clothes and underwear made of cotton and natural fibers that are loose, cool and breathable.
Do not clean your vagina with vaginal douches, but only wash its exterior and vulva;
Avoid shower gels, soaps, sprays and deodorants for the intimate area that contain perfume, dyes, parabens and other chemicals that can irritate your skin;
Use only water and a natural pH-neutral intimate gel to maintain your vulvovaginal hygiene - Enroush intimate gel is specially formulated to protect your genital area with 95% natural ingredients.
Protect yourself from sexually transmitted diseases and other infections by using a condom with every sexual contact;
Use only organic menstrual products that let your skin breathe and keep it dry without causing irritation. Enroush absorbent pads and tampons are made from 100% GOTS certified organic cotton and contain no plastic, fragrances, dioxin or synthetic fibres.

Go to a gynecological consultation periodically to detect any type of infection early, including asymptomatic ones.
Vulvovaginitis in children
Girls, especially in the period before and during puberty, are prone to vulvovaginitis because their vaginal environment is more alkaline, without vaginal secretions, and the vulvo-vaginal mucosa is much thinner. So if in an adult woman, the main causes are infections with various viruses, bacteria and microorganisms transmitted through sexual contact, in children vulvovaginitis occurs mainly due to mistakes in maintaining proper hygiene.
This means both poor and excessive hygiene. It can occur in girls of all ages, from infancy, if diapers irritate her, to puberty. Especially if the hygiene is insufficient or the intimate area is not wiped properly, the bacteria will remain there and favor the occurrence of inflammations and infections.
Other causes of vulvovaginitis in children include excessive use of wet wipes, wearing underwear that is too tight, using detergents or conditioners with harmful chemicals when washing underwear and clothes, increased humidity in the intimate area or the use of shower gels, soaps or of bath foams with perfumes and other skin-invasive ingredients.
The symptoms of vaginitis in girls are mainly swelling of the vulva and vagina, redness and the appearance of burning sensations, itching, stinging when urinating and an unpleasant smell. After the doctor makes this diagnosis according to the signs of the condition, the treatment will be done primarily by eliminating the source of the irritation, and depending on the severity, by administering antibiotics.
To prevent this problem from appearing in the girl's life, the most important thing is for parents to pay close attention to her hygiene, and as she grows up, teach her how to wipe herself properly, how to wash herself properly and how to protect herself of infections and irritations. These preparatory steps are essential so that the girl is ready to properly maintain her own hygiene as she approaches puberty and desires more and more privacy. I have blogged about this time full of changes in a woman's life before, so we invite you to read there a lot of other useful information about puberty in girls .
Vaginitis in pregnancy
According to some studies, bacterial vaginitis is one of the most common problems of the genital tract that pregnant women face. There are statistics that claim that between 10% and 30% of women develop this condition during pregnancy, mainly due to the hormonal changes that occur during this period.
The most common and obvious symptom of vaginitis in pregnant women is the unusual, pungent odor in the intimate area, but there are also cases in which watery gray discharge, burning sensation when urinating or itching in the vulvovaginal area also occur. Bleeding is not among the common symptoms of vaginitis in pregnancy, but it can indicate other health problems. So if you are pregnant and notice unusual bleeding, the information we have prepared for you about bleeding in pregnancy may help you.
The greatest risk of bacterial vulvovaginitis during pregnancy is premature birth and low birth weight. Both can create other health problems for the baby later. Equally dangerous are vaginitis caused by sexually transmitted diseases, because these diseases can be transmitted from mother to fetus before, during and even after birth.
The doctor can prescribe a course of antibiotics, which are safe for the baby, treat bacterial vaginitis and can reduce the risk of sexually transmitted diseases. They can be administered orally in the form of pills, or they can be applied locally in the form of a gel or cream.
It is preferable to avoid them, however, because antibiotics can also kill the good bacteria inside the vagina. An alternative treatment, if the antibiotic is not absolutely necessary, could be vaginal probiotics. They contain the right doses of micronutrients (iron, manganese, zinc) that help restore a healthy vaginal flora, so that your vaginal balance is no longer disturbed during pregnancy.






















