
Ovarian Cysts - What are they? Symptoms, Causes & Treatment
Conditions that affect your uterus or any other part of your reproductive system are called uterine problems. Some common uterine problems include ovarian cysts, uterine fibroids, endometriosis, uterine prolapse, and uterine tuberculosis.
What is an ovarian cyst?
An ovarian cyst is a sac filled with liquid or semi-solid material that forms on or inside one or both ovaries. The ovaries are small organs in the pelvis that contain eggs and produce hormones such as estrogen and progesterone.
There are different types of ovarian cysts, most of which are painless and harmless (benign). Usually, ovarian cysts are not felt through specific symptoms. You probably won't know you have one unless your doctor discovers it during a routine pelvic exam or imaging procedure.
Rarely, ovarian cysts can cause complications. Scheduling regular pelvic exams and talking to your health care provider about any symptoms you may be experiencing can help prevent your health from deteriorating. Ovarian pain for no apparent reason can be a sign of an ovarian cyst that can cause complications. (read more on the ENROUSH blog )
Ovarian cyst - Symptoms
An ovarian cyst usually only causes symptoms if it ruptures, is very large, or blocks blood flow to the ovaries.
In these cases, you may experience the following symptoms:
pelvic pain – this can range from a dull sensation to a sudden, severe, sharp pain
pain during intercourse
difficulty emptying your bowels
frequent need to urinate
heavy, irregular or lighter-than-normal periods (find out when to worry if you notice irregular bleeding in our article )
bloating and a swollen belly
feeling full even if you have eaten very little
difficulty getting pregnant – although fertility is usually unaffected by ovarian cysts
Types of ovarian cysts
There are three main types of ovarian cysts, and each of these can have a number of subtypes.
Functional ovarian cysts
Functional ovarian cysts are those cysts that develop as part of the menstrual cycle. They are usually harmless and short-lived, occurring frequently in women of all ages.
Ovarian follicular cyst
Halfway through the menstrual cycle, an egg is released from its follicle. It then moves along a fallopian tube. A follicular cyst begins when the follicle does not rupture. He does not release the egg and continues to grow. Most follicular cysts are painless and harmless. They are not cancerous. Fortunately, these cysts often disappear on their own within a few menstrual cycles. Most of the time you won't even notice that you have a follicular cyst.
Luteinous ovarian cyst
After a follicle releases its egg, it shrinks and begins to produce estrogen and progesterone. These hormones are necessary for conception. The follicle is now called the corpus luteum or yellow body. Sometimes the opening where the egg came from ends up getting blocked. Fluid builds up inside the corpus luteum, causing a cyst. Most of the time they disappear spontaneously within a few months, but sometimes they can break, causing complications.
Hemorrhagic ovarian cysts
Hemorrhagic ovarian cysts are those that develop in ovulating women when a follicle bleeds and develops a fluid-filled sac around it (a follicular or corpus luteum cyst). They are not uncommon, but only occur in women of reproductive age. They can grow to different sizes, from very small to quite large. Although most cause no symptoms at all, some hemorrhagic ovarian cysts can cause problems such as abdominal or pelvic pain, pressure, and a constant feeling of fullness.
Pathological ovarian cysts
There are a number of other types of ovarian cysts that are not related to the menstrual cycle. These are called pathological ovarian cysts.
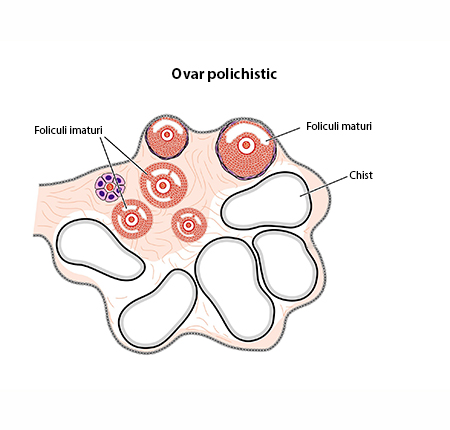
Polycystic ovary syndrome
Polycystic ovary syndrome (PCOS) is a condition in which the ovaries produce an abnormal amount of androgen, male sex hormones that are usually present in women in small amounts. The name polycystic ovary syndrome describes the many small cysts that form in the ovaries. This condition can cause several problems with a woman's menstrual cycle, which can have a negative impact on fertility. Treatment for PCOS is often done with specific medications. It cannot completely cure PCOS, but it helps reduce symptoms and prevent more serious health problems.
Ovarian dermoid cyst
Also called a teratoma, this cyst forms from the reproductive cells that produce eggs in the ovary (germ cells). The cyst may also contain tissue such as hair, skin or teeth. This type of cyst is rarely cancerous. It requires surgery to be removed and occurs most often in women under the age of 30.
Endometriosis ovarian cyst
Endometriosis is a condition that causes cells similar to those lining the inside of the uterus to grow outside the uterus. This type of tissue can attach to the ovary, forming a cyst. It is called an endometrioma. Although often asymptomatic, endometriotic ovarian cysts can cause pain during menstruation or intercourse.
cystadenoma
Cystadenoma is formed from the cells that form the surface of the ovary. The cyst usually fills with either watery or mucilaginous material.. A cystadenoma can grow very large, potentially causing complications. Although it will rarely be malignant, this cyst requires surgery to be removed. It is most common in women over 40 years of age.
How do ovarian cysts affect menstruation?
Ovarian cysts can also lead to problems with your menstrual cycle, such as heavy or irregular periods and spotting (abnormal vaginal bleeding between periods). Menstrual cycle problems occur if the cyst produces sex hormones that cause the lining of the uterus to develop more than it should. In these cases it will be useful to switch to menstrual protection with a higher degree of absorption and use protective panties between periods.
ENROUSH pads and tampons have three levels of absorbency, perfect for any fluctuations in your flow during your period. Moreover, they contain 100% organic cotton and natural fibers, being gentle on the skin and reducing vaginal discomfort. If your ovarian cysts have severe menstrual cramps as a side effect, ENROUSH thermal patches are a quick, natural and effective pain reliever.

Risk factors - Ovarian cysts
There are a number of risk factors that increase the likelihood of developing ovarian cysts:
Hormonal changes. These include taking a fertility drug that makes you ovulate, such as clomiphene or letrozole (Femara).
Task. Sometimes the follicle that forms when you ovulate stays on the ovary throughout the pregnancy. It can grow in size, thus developing a cyst
Endometriosis. Some of the tissue can attach to the ovary and form an endometriotic ovarian cyst.
Severe pelvic infection. If the infection spreads to the ovaries, it can cause cysts.
Previous ovarian cysts. If you've already had one ovarian cyst, you may develop more.
When should you go to the doctor?
Most of the time, ovarian cysts are uncomplicated and can go away on their own. Sometimes, you won't even know you have them unless they were diagnosed during a regular medical exam. However, those that cause physical symptoms and continue to grow uncontrollably require closer monitoring.

Make a list of all the symptoms you have so you can tell your gynecologist about them. Follow his advice on how often you should make appointments to monitor any cysts. Regular medical examinations can prevent cysts from getting worse or other serious health problems.
Contact your gynecologist if you have any of the following symptoms:
Menstruation is late, irregular or painful.
Abdominal pain does not go away.
Your abdomen becomes enlarged or swollen.
You have problems urinating or emptying your bladder.
You have pain during intercourse.
You have a feeling of fullness (bloating), pressure or discomfort in your abdomen.
Lose weight for no apparent reason.
You have a general malaise
You have severe abdominal pain that comes on suddenly, accompanied by vomiting or fever.
Diagnosis of ovarian cysts
An ovarian cyst may be found during a pelvic exam or an imaging test, such as a pelvic ultrasound. Depending on its size and whether it is filled with liquid or has a solid consistency, the doctor will recommend a series of tests to determine its type and whether treatment is needed.
Possible tests include:
Pregnancy test. A positive pregnancy test may be a sign that you have a lutein cyst.
Pelvic ultrasound . A wand-like device sends and receives high-frequency sound waves to create an image of the uterus and ovaries on a video screen. The image is used to confirm that you have a cyst, see its location, and determine whether it is solid or fluid-filled.
Laparoscopy. A thin, lighted instrument (laparoscope) is inserted into the abdomen through a small cut (incision). Using the laparoscope, the doctor can see your ovaries and any potential cysts. If a cyst is found, treatment is usually done during the same procedure. This is a surgical procedure that requires anesthesia.
Tests with tumor markers. Blood levels of a protein called cancer antigen are often elevated in ovarian cancer. If the cyst appears solid and you are at high risk for ovarian cancer, your doctor may order a cancer antigen 125 (CA 125) test or other blood tests.
Ovarian cyst treatment
Depending on the cyst, its size and type, the gynecologist may suggest different invasive or non-invasive treatments.
Ovarian cyst medicinal treatment
Hormonal contraceptives, such as birth control pills, prevent ovulation. This can stop more ovarian cysts from forming. Birth control pills will not shrink an existing cyst, but can be used as an adjunctive treatment.
Ovarian cyst operation
Your gynecologist may suggest surgical removal of a cyst that is large, growing, or causing pain. This type of treatment is also used for abnormally shaped cysts. Some cysts can be removed without damaging the ovary (cystectomy). In some cases, the ovary is removed completely (oophorectomy) to treat the problems caused by the ovarian cyst.
The intervention can often be done using minimally invasive surgery (laparoscopy) with a laparoscope and instruments inserted through small cuts in the abdomen. If the cyst is large or cancer is a concern, an open procedure using a larger incision may be necessary.
An ovarian cyst that develops after menopause can sometimes be malignant. In this case, it is necessary to consult a specialist in gynecological cancer. You may need surgery to remove your uterus, cervix, fallopian tubes, and ovaries. For malignant cysts, radiation therapy and chemotherapy may also be necessary.
Can the ovarian cyst be treated with natural remedies?
Natural remedies cannot treat a cyst that needs monitoring and surgery. It is always good to follow the advice of the specialist regarding effective treatment methods for gynecological conditions.
However, for small cysts that are not a cause for concern, chamomile and ginger teas may relieve some symptoms such as pain or bloating. Massage and light exercise can also reduce the intensity of menstrual cramps made worse by cysts.
Furthermore, a balanced diet rich in fruits, vegetables and whole grains has a beneficial effect on overall health and may help prevent ovarian cysts.
Sexual life after ovarian cyst surgery
Libido is an incredibly personal thing that a large number of factors can affect. So it makes sense that surgery on your reproductive organs could have a significant impact. Oophorectomy is a major surgical procedure, so it's perfectly normal to not feel ready to have sex for a certain period of time. It is important to give yourself time to recover both physically and mentally.
If you had an oophorectomy along with a hysterectomy, you may find that you enjoy penetrative sex less than before. This new preference may be because the surgery has changed the position and length of the vagina, although this is not always the case.
The most important thing is to follow any advice from your doctor about sex and other physical activity after surgery. Most women who have had oophorectomies enjoy a healthy sex life after recovery. However, it is good to remember that the removal of one or both ovaries also has an effect on libido, as it leads to a decrease in the level of hormones that directly affect it.
Complications - Untreated ovarian cyst
Many ovarian cysts go away on their own. However, some of them require specialized treatment. If left untreated they can lead to certain complications such as:
Ovarian torsion: Cysts that become large can cause the ovary to move. Because of this there is an increased chance of the ovary twisting painfully (ovarian torsion). If this happens, you may experience sudden and severe pelvic pain, along with nausea and vomiting. Because of this condition, blood flow to the ovary can be reduced or even stopped.
Cyst Rupture: A cyst that ruptures can cause severe pain and bleeding inside the pelvis. Large cysts have an increased risk of rupture. Vigorous activity that affects the pelvis, such as vaginal sex, also increases the risk of rupture.
Prevention of ovarian cysts
There is no way to prevent most ovarian cysts. However, regular pelvic exams help ensure that ovarian changes are diagnosed as early as possible. Be aware of changes in your menstrual cycle. Note unusual menstrual symptoms, especially those that last more than a few cycles. Talk to your gynecologist about any unusual changes that raise questions.
Also, a number of lifestyle changes can reduce the risk of ovarian cysts:
Maintain a normal body weight
Avoid taking fertility drugs as much as possible
Avoid alcohol and tobacco
With the doctor's approval, certain contraceptive methods that contain hormones can be a preventive treatment for the appearance of cysts






















