
Hormonal acne is usually associated with adolescence, when it is said (I'm sure you've heard this saying) that "hormones go crazy". It also occurs in adults, where acne based on hormonal fluctuations mainly affects women, because we face a lot of factors that influence our hormonal balance, including menstruation and menopause.
We know it's unpleasant, we know it affects us especially in those few days before menstruation. But what can we do to keep it under control and enjoy smooth skin? Let's see how hormonal acne is defined, why it occurs and how we take care of our skin to avoid it.
What is hormonal acne?
Hormonal acne is not a medical term, but just a name we use in popular language when we simply refer to acne.
However, we have a reason to call it that, because it is found especially during puberty or before menstruation. For this reason, it is associated with the hormonal changes that occur during this period.
Acne is actually related to excessive sebum production that leads to clogged pores, causing inflammation and pimples. Sebum production which, in turn, is influenced by hormonal fluctuations in the body - hence the name.
Who does hormonal acne affect?
Anyone can be affected by hormonal acne, from teenagers who are prone to this skin condition to adults between the ages of 10 and 50.
Acne occurs in both women and men, but cases are more common in women, especially pregnant women and those reaching menopause.
How common is hormonal acne?
We know that acne is among the problems that can affect your confidence and self-image the most - it's a problem that many teenagers face, especially girls at puberty . But it's more normal than you'd expect.
Acne is the most common skin condition. Statistics estimate that it affects about 50% of women between the ages of 20 and 29 and 25% of women between the ages of 40 and 49.
Hormones responsible for the appearance of acne
Several hormones are involved in acne. A 2016 study identified estrogen, progesterone, androgens, insulin, cortisol, and growth hormone (GH) as among the hormones that have a significant impact on acne. (PMID: 27621661)
Changing the level of any of these hormones in the body can lead to pimples:
Androgens: Sebaceous glands increase in response to changes in testosterone, androstenedione and dihydroepiandrotension (DHEAS) levels
Estrogen: inhibits testosterone production and increases the secretion of sex hormone-binding globulin (SHBG), acting at the level of hair follicles, hairs and sebaceous glands (called the polysebaceous unit)
Progesterone: Progesterone receptors are found in keratinocytes in the basal layer of the epidermis, leading to increased sebum production and supporting pre/menstrual breakouts.
Insulin: is related to insulin-like growth factors (IGF-1) and can increase androgen and sebaceous gland production
GH: growth hormones have receptors in follicles and sebaceous glands that will directly respond to fluctuations
CRH: are the hormones that release corticotropin and inhibit the multiplication of sebaceous glands, contributing to the conversion of dihydroepiandrotensin (DHEA) to testosterone
Cortisol: stress hormones (glucocorticoids) stimulate the multiplication of sebaceous glands
Normally, estrogen, progesterone and testosterone fluctuate throughout the menstrual cycle, hence the worsening of acne in menstruating, menopausal and pregnant women.
Likewise, if you use or stop using hormonal contraception (eg birth control pills), there may be large hormonal fluctuations responsible for skin rashes.
But acne can also be an effect of hormonal fluctuations that occur when a hormonal problem occurs in the body. Polycystic ovary syndrome (PCOS), tumors (ovarian, pituitary, adrenal or hypothalamic) or congenital adrenal hyperplasia, all of these can affect the production of the hormones we told you about, producing imbalances and influencing the sebaceous glands. You can read more about hormonal disorders HERE .
How hormonal acne occurs and develops
Hormonal acne occurs due to clogged pores. But until this happens, we can divide the acne development process into four stages:
Hormones fluctuate: due to increased testosterone production or hormonal changes during menstruation, the body secretes more sebum.
Sebum clogs pores: Excessive sebum in the skin leads to clogging of hair follicles and thus whiteheads or blackheads are formed.
Bacteria causes an infection: When the pores are clogged, the bacteria on the surface of the skin gets stuck there and causes an infection that causes painful pimples.
Inflammation occurs: the body's immune system activates in response to the bacterial infection, causing the site to redden and swell, and papules, pustules, nodules, and cysts may appear.
Depending on how the bacteria spreads and the skin continues to become inflamed, acne can spread:
On the T-zone of the face (forehead-nose-chin)
On the jawline and cheeks
On the neck, shoulders, chest, back

Causes of hormonal acne that you can control
You cannot control how the hormones in your body change in response to natural functions such as puberty, the menstrual cycle, or menopause. But there are factors that can make acne worse and hormonal fluctuations that you can control:
Stress: When you don't manage your heavy periods, stress increases cortisol and androgens in the body, which leads to more sebum production. Try practicing relaxation and stress management techniques to avoid these situations.
Lack of sleep: Likewise, when you don't get enough rest, your body doesn't have time to recover and doesn't control your cortisol levels as well. More sebum, more clogged pores, more pimples. Try to get at least 7 hours of rest per night.
Using the wrong products for the skin/hair: especially products rich in oils (greasy face creams, shampoos containing essential oils) but also cleaning gels with allergens can clog the pores from the outside, blocking bacteria there and leading to inflammation. Opt for products as natural as possible, made from hypoallergenic ingredients with a neutral pH and safe for acne-prone skin.
Causes of hormonal acne that you can't do anything about
Unfortunately, there are also factors that you can't really influence. Among the causes of hormonal fluctuations that lead to acne and about which there is not much you can do, we find:
Hormonal changes in women: Estrogen and progesterone naturally fluctuate throughout the menstrual cycle, during pregnancy and perimenopause
Testosterone treatments: Testosterone supports sebum production, so men on testosterone treatments are prone to hormonal acne
Genetic predisposition: if you have family members who suffer from acne, there is an increased risk that it will affect you too
Side effects of certain drugs: steroids, for example, or birth control pills, cause hormonal changes that can lead to acne
Certain medical conditions: When you suffer from ovarian conditions or metabolic problems, there are also hormonal imbalances that can cause you to experience acne. One such cause is polycystic ovary syndrome, about which I told you everything you need to know HERE .
Risk factors of hormonal acne
I told you above about the most common causes of hormonal acne, but there are several other risk factors that can trigger it. The predisposition increases with:
- Psychological and emotional stress (can produce neuropeptides that trigger skin inflammation)
- Genetic factor (affects the number of sebaceous glands and how they secrete sebum)
- External factors (medicines, care products, hormonal treatments)
- Exposure to certain environmental conditions (pollution, humidity)
- Harmful habits (nicotine and benzopyrene in the case of smoking)
- Improper treatment (squeezing pimples that spread acne bacteria)
- Diet (an unbalanced diet is not a direct cause of acne, but it is a risk factor that worsens the condition if it already exists)
Hormonal acne - Symptoms
Hormonal acne most often affects the skin of the face, and can spread to the neck, chest, shoulders and back. The specific symptom is the inflamed appearance of the skin, in the form of pimples. They may be accompanied by redness, swelling, itching and sensations of stinging, stinging or pain.
Hormonal acne can manifest itself in the following forms:
White dots
Black dots
Papules (bumps on the skin)
Pustules (bumps containing pus)
Cysts (formations under the skin that contain fluid)
Even after treating inflammation, the skin may remain with post-acne symptoms such as:
Hyperpigmentation
scar
How is hormonal acne diagnosed?
Hormonal acne is not, as we said above, a medical term, but rather a common name for acne. Therefore, the diagnosis will be made only for acne, following an evaluation made by the doctor.
In addition to the visual examination of the inflammations, the dermatologist may also ask you:
- If you use any kind of medicine
- If there have been hormonal or health changes
- How much you rest and what sleeping habits you have
- If you are going through a stressful time
- What products do you use for skin/hair care?
Sometimes an endocrinological consultation may also be needed, to determine if there are problems of a hormonal nature.
Depending on the appearance of the skin and the severity of the symptoms, the dermatologist will be able to diagnose the acne and its degree of severity, starting from mild to very severe.
Treatment for hormonal acne
Acne is treated in the long term. We're not just talking about a treatment, we're talking more about a care ritual that your skin will need on a daily basis. Although pimples may disappear after using various solutions, there are very high chances that they will reappear if you later neglect this aspect.
This is not to say that we equate acne with carelessness about your skin or lack of care. It is a myth that hormonal acne occurs due to poor hygiene. But there are little habits you can add to your skincare routine to keep breakouts under control and inflammation to calm down. And if you give them up and don't pay as much attention to the products you use, the skin is still prone to acne and relapse is possible.
Thus, you keep acne under control in two ways: treatment and care routine.
When it comes to treating pimples, the severity of your acne, how your skin has responded to treatments you've tried before, and whether you're pregnant or suffering from hormonal imbalances will all be taken into consideration. The alternatives are many and varied, including:
Tretinoin creams and gels for external use: for whiteheads and blackheads
Creams and other topical treatments with retinoids, antibiotics, benzoyl peroxide: to treat inflammation caused by acne
Antibiotic or isotretinoin: to treat moderate/severe acne
Steroid injections: to treat cystic acne
Hormonal therapy or contraceptives: to restore hormonal balance, when there is an endocrinological disease or acne does not disappear after using treatments for external use (only on the recommendation of the gynecologist/endocrinologist)
Other procedures: extraction, chemical peels, laser treatments and other interventions on the skin, when acne is severe, does not respond to local treatments or scars remain
Acne skin care does not end with treatment, however. At the same time, and even after it's over, here are some recommendations for your skin care routine that will help you prevent further breakouts:
Do not use natural treatments without the advice of a dermatologist: natural treatments sound promising because they contain natural ingredients, but acne skin is very sensitive, and you risk exposing it to substances that can cause contact dermatitis and other side effects. Always ask your dermatologist for advice before using any treatment.
Choose your cosmetics carefully: use sunscreens, cleansers and other products, but always check the label. Choose products that are as natural as possible, without allergens, compatible with sensitive skin and that do not contain oils that can worsen sebum production.
Avoid squeezing pimples: We know it's tempting sometimes, but all you're doing by squeezing is spreading acne bacteria further into your skin pores.
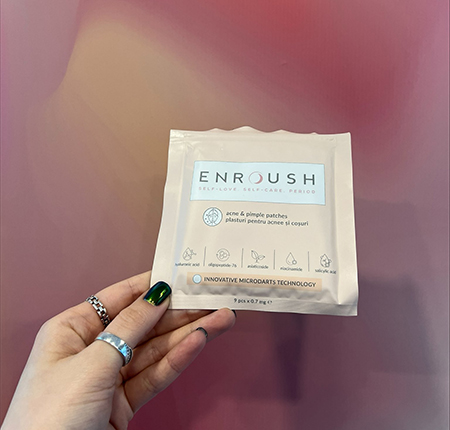
Use Enroush Pimple and Acne Patches : They are a much more effective solution than squeezing. You just miss it on the skin and the micro arrows will drive the unique mix of active ingredients deep, treating pimples from the root in just 6 hours. Thanks to salicylic acid, hyaluronic acid, niacinamides and oligopeptide-76, the patches cleanse, extract and hydrate the skin, leaving it smooth and clean without scars or signs of aging.
Adjust your diet: even if it is not a direct and proven cause of acne, diet plays an important role in establishing the hormonal balance in the body and can be a risk factor. When you notice that certain foods create inflammation (ex: excess sugar or processed foods), try to limit their consumption.
Complications of hormonal acne
Hormonal acne does not have serious health complications, but there are several ways we can look at its long-term effects.
In terms of physical appearance, the most common complications of acne are scarring and hyperpigmentation that occur after the inflammation subsides and the pimples disappear. The marks may remain on the skin for a long time or permanently if the acne was severe.
A perhaps even more serious long-term effect is on the emotional state, because acne often has a strong negative impact on self-image and social life. People affected by acne often face bullying, discrimination, and feelings of shame, low self-esteem, isolation and depression.
Also, if acne hides a hormonal imbalance and an endocrinological problem, complications of that disease may occur if not properly treated. So it is good to do more investigation when there are suspicions.
How to prevent hormonal acne
Nothing can guarantee the prevention of hormonal acne with certainty, because you cannot precisely control the changes in the body and the way hormones fluctuate. Especially when we talk about normal functions such as the menstrual cycle, pregnancy or menopause.
But you can certainly take steps to limit risk factors, so you can protect your skin and treat acne as quickly as possible from the first signs:
Pay attention to your lifestyle: diet, rest, stress level, all these have a major impact on hormonal balance and sebum production. Give yourself nutritious food, get enough sleep and avoid stressful situations as much as possible.
Use hypoallergenic skincare products: Cleanse your skin daily, but make sure you use products that don't clog pores and increase the risk of inflammation.
Go to the dermatologist: make regular visits if you know you have a genetic predisposition to acne, and ask for a doctor's recommendation at the first signs of acne, before the severity increases
Discuss treatment options with your doctor: for persistent or recurring acne, ask your dermatologist what other solutions are available
Hormonal Acne FAQs
We don't want to leave you with unanswered questions, and we know that acne can raise many questions. How does it affect you? How long do the rashes last and how long does it take for the treatment to take effect? We listened to the most frequently asked questions about hormonal acne and prepared the answers here:
How does hormonal acne affect my skin?
Breakouts are the central symptom of acne. The skin may redden and lesions or pimples (blackheads, whiteheads, pustules, nodules) with an inflamed appearance may appear, which may itch, sting, sting or hurt. After treating severe acne, scars may also remain on the skin.
How long does hormonal acne last?
The answer differs from person to person. If it is caused strictly by certain hormonal disturbances, it may disappear after the balance is restored. Some pimples disappear in just a few days. More serious forms can last several weeks. Without treatment, acne may persist for months.
How soon after treatment will hormonal acne go away?
Likewise, each person's experience is different. Every body is unique and responds differently to various forms of treatment. Acne means long-term therapy, so you have to be patient. Symptoms should improve within six weeks of starting treatment, but always talk to your dermatologist for realistic expectations.
Do I need to see a dermatologist to treat my hormonal acne?
Yes, it is always recommended to seek the advice of a specialist doctor. Do not choose to self-medicate or ignore the problem, because it can get worse. You never know what adverse reactions can occur when your skin comes into contact with various substances, and it is best to follow the dermatologist's instructions. He will prescribe a suitable treatment depending on the severity of your acne and your health.






















