
Cervical cancer - Evolution, Risk Factors, Diagnosis & Treatment
Cervical cancer is considered one of the main causes of cancer mortality in women in Romania. Unfortunately, the medical, educational and political system, as well as the mass media, are not very helpful when it comes to awareness of the importance of screening - essential in cancer prevention. The HPV test and Pap test are vital in maintaining a woman's health, but too few people do them on time or regularly, and that's because of the system that doesn't encourage us.
So, we chose to write about cervical cancer so that you can have more information and find out everything you wanted to know, from the anatomy of the uterus to symptoms, risk factors, diagnosis and treatments. Read on!
Cervical cancer - What is it?
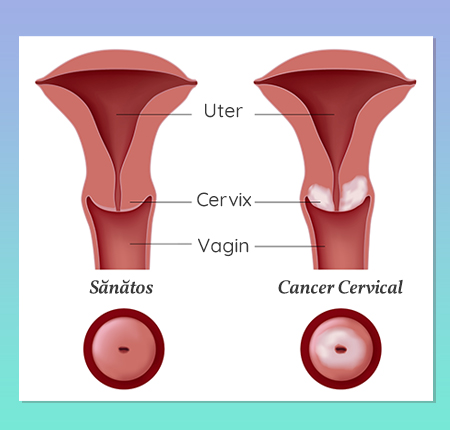
Cervical cancer occurs at the level of the cervix, that is, the lower part of the uterus that connects to the vagina. The cervix consists of two different parts and is covered with two types of cells:
Endocervix: the part of the cervix next to the body of the uterus, covered with glandular cells.
Exocervix or ectocervix: the part near the vagina, covered with squamous cells.
Cervical cancer - Symptoms
When at the level of the cervix, atypical cells multiply uncontrollably, cervical cancer occurs. At an early stage, changes in the cervix are often without symptoms. So, cervical cancer can only be diagnosed and identified through regular check-ups!
In an advanced stage, you may have symptoms such as:
heavy bleeding and pelvic or lower back pain
vaginal secretions with an unpleasant smell
pain during intercourse and/or bleeding after sex
Anemia
Sudden and significant weight loss in a very short time
Menstruation with cervical cancer
Although heavy periods are usually signs of conditions such as endometriosis, they, especially when they are long-lasting, can be associated with symptoms of cervical cancer. A heavy period lasts more than 7 days in which you need to change the absorbent / tampon every 2-3 hours. This condition can be caused by irritation of the cervix, so it is essential to see a gynecologist.
Hormonal imbalances and harmful substances in intimate hygiene products can cause heavy or irregular periods, so always make sure you use 100% organic cotton pads with no hidden ingredients.
Causes of cervical cancer
Cervical cancer develops from precancerous changes, present for many years in the body, and the most common cause is HPV (Human Papillomavirus) infection - more than 90% of cervical cancer cases. But what you need to know is that even if you have an HPV infection, in most cases it does not cause cervical cancer. Prevention is vital and regular screening and testing every year is absolutely necessary to prevent cervical cancer.
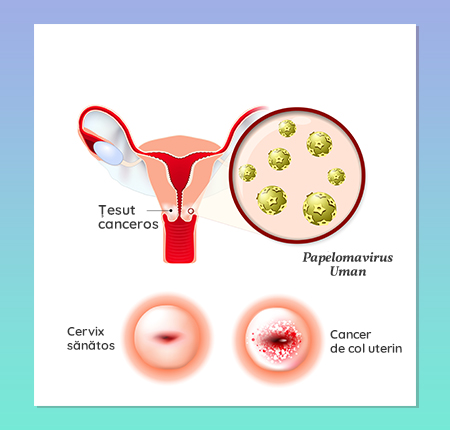
The HPV virus affects the mouth, throat or genital area. So sexual contact is not the only way HPV is transmitted. In fact, the virus can be transferred through a cut, an abrasion of the skin, or simply through skin-to-skin contact. What's more, a person with HPV can pass the infection on to someone even if they don't have symptoms. You can contract HPV by:
any skin-to-skin contact of the genital area
vaginal, anal or oral sex
sex toy exchange
Symptoms can appear years after contact with the virus, which complicates things when you want to find out the exact cause and when you came into contact with the virus.
Read more about HPV in an article dedicated to this topic.
Risk factors - HPV & Cervical Cancer
As for the risk factors, they are diverse. Some of the most common factors identified include:
HPV infection
HSV 2 genital herpes infection
HIV/AIDS infection
Chlamydia infection
Poor hygiene of sexual partners
History of sexually transmitted infections and diseases
long-term administration of oral contraceptives
PS: The risk of cervical cancer increases as you use birth control pills for more than 5 years! Read all about birth control here.
Smoking
Immunosuppression
Deficiency of vitamins and minerals in the daily diet
Overweight
Multiple tasks
Types of cervical cancer
There are several types of cervical cancer, including:
squamous cell (epidermoid) cancer diagnosed in 75% of women with malignant lesions)
cervical adenocarcinoma
mixed cervical carcinomas
other malignant tumors with cervical involvement
Squamous cell carcinoma
Squamous cell carcinoma accounts for approximately 85% of all cervical cancers. It develops in the cells of the scaly-looking exocervix in the outer region of the cervix, which projects toward the vagina.
Adenocarcinoma
Adenocarcinoma accounts for about 10-15% of all cervical cancers and develops from mucus-producing glandular cells in the endocervix.
Mixed carcinomas
Less common are mixed carcinomas, which have features of both squamous cell carcinomas and adenocarcinomas.
Evolution of cervical cancer
The place where these two types of cells meet in the cervix is called the transformation zone. The exact location of the transformation zone changes as you age and due to changes such as pregnancy and childbirth.
These cells in the transformation zone do not suddenly turn into cancer. Instead, the normal cells of the cervix first gradually develop abnormal changes called pre-cancerous changes.
And although cervical cancers start from cells with precancerous changes, only some of the women who have them will develop cancer. That's why it's important to have regular check-ups and not to skip the Pap test every year. For most women, pre-cancerous cells will disappear without any treatment. Your gynecologist can recommend treatment if needed. If they are not treated, they can turn into invasive cancer, which will have several stages.
Stage 0 - Carcinoma in Situ
Stage 0 of cervical cancer means damage to the first layer of cells of the cervix, without invasion into the deeper layers.
Stage 1 - Tumor only in the cervix
Stage 1 has two phases:
1a is when the cancer does not invade the cervical tissue more than 5mm in depth and is not larger than 7mm.
1b is when the cancer invades the cervical tissue in depth more than 5 mm and is greater than 7 mm.
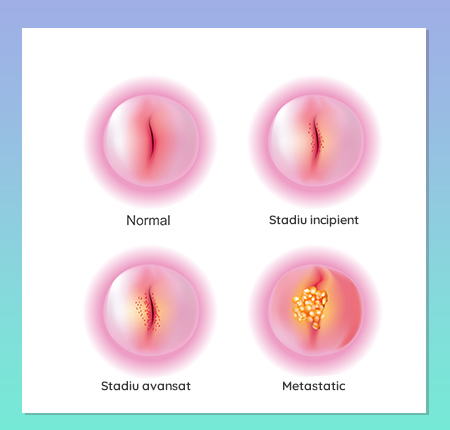
Stage 2 - The cancer has spread to the vagina
In stage two cervical cancer, the condition spreads and affects the upper two-thirds of the vagina, but not the pelvic wall. And here there are two stages:
Stage 2a which represents an invasion of the vagina and
Stage 2b which represents an invasion beyond the upper two thirds of the vagina.
Stage 3 - The cancer covers the entire vagina
In the 3rd stage, the cancer invades the lower third of the vagina, in two phases:
Stage 3a, in which the condition does not also invade the pelvic wall
Stage 3b where the cancer invades the pelvic wall and/or is large enough to block the ureters.
Stage 4 - Cancer invades other parts of the body
Even before it invades other parts of the body, cancer can spread to the pelvic area. This is how stage 4 cancer begins.
In stage 4a, it can affect the bladder and rectal wall or lymph nodes in the pelvis.
In stage 4b, it can spread to distant organs outside the pelvic area, such as the lungs or bones.
Cervical cancer diagnosis
In the early diagnosis of cervical cancer, screening tests are most important. Through them, your doctor can detect pre-cancerous lesions in time, which can be treated. Screening is recommended to start at age 21.

Gynecological examination
Annual gynecological examination is important and essential in detecting any problems and potential complications. As part of the consultation, the doctor will recommend certain tests and consultations to determine possible conditions.
Pap test
The Babeș Pap test is one of these tests, and the most important. It consists in collecting some cells from the exocolus that will be analyzed microscopically to identify any abnormal, pre-cancerous or suspicious cells. But it is not the only test that must be performed for a diagnosis.
Colposcopy
Your gynecologist may recommend colposcopy, an investigation that evaluates the vagina and cervix. This can be done with or without a biopsy, including if you are pregnant. It is not painful, in fact, it is like any other examination such as the Babeș-Papanicolau test. It is recommended to do it before or after your period, not during bleeding.
Cervical biopsy
Then there's the cervical biopsy. If the biopsy results confirm cervical cancer, your gynecologist may request additional tests to see how extensive it is: ultrasound, computed tomography, MRI, PET. The next step is the staging of the disease.
Cervical cancer - Life expectancy
Globally, approximately 570,000 women are diagnosed with cervical cancer each year, and it is the fourth leading cause of cancer death after breast, lung and colorectal cancer.
Of the total number of cervical cancers diagnosed annually in Europe, 7.5% come from Romania, and the mortality rate is 4 times higher than the European Union average, unfortunately.
But then cervical cancer can be successfully prevented and treated by the most effective method: regular check-ups at the gynecologist and HPV testing as well as the Babeș-Pap test, once a year. The first PAP test should be performed within a maximum of 3 years from the start of sexual life, but no later than the age of 21.
Cervical cancer - treatment
Treatment for cervical cancer is determined by the doctor, depending on the stage of the cancer and other factors that can influence the treatment, including general health, age, preferences of each person - because this disease affects fertility and sex life.
So, the treatment can be in the form of:
A surgical intervention
Radiotherapy (X-rays to destroy cancer cells)
Chemotherapy (substances that destroy tumor cells)
Targeted therapy
Cervical cancer surgery
In the case of surgical interventions, they can be of several types and help both to diagnose cervical cancer, to assess the stage, but also to treat the cancer, especially if it is in an early phase. Depending on the patient, the doctor can recommend a type of surgery, such as: cryosurgery, laser surgery, conization, total hysterectomy, radical hysterectomy, trachelectomy.
Chemotherapy
Chemotherapy is the method by which substances are administered with the aim of destroying cancer cells. This can be given orally or intravenously. The doctor will establish the doses and the treatment, to be as effective as possible in the specific symptoms.
Radiotherapy
Radiotherapy uses high-intensity beams of radiation and may be given in combination with chemotherapy in advanced stages. It can also be recommended after the operation, if the doctor deems it necessary. Radiotherapy can be administered:
Externally, by directing radiation beams to the affected area
Internally, by placing a device with radioactive content (eg in the vagina)
Combined, both internal and external
Drug treatment
In the case of cervical cancer at an advanced stage or if the cancer has recurred, the specialist doctor may recommend a drug treatment with a precise target. The purpose of this medicine is to help shrink the cancer or stop it from spreading. So the targeted therapy will inhibit the mutations that favor the multiplication of cancer cells.
Recovery after cervical cancer
After cervical cancer, palliative care plays an important role in providing support, controlling symptoms and helping you improve your quality of life when you have had cancer.
Moreover, once the treatment is finished and the healing process begins, it is recommended to go for a check-up every 3 months for the first 2 years. Afterwards, this consultation can be done every 6 months.
How can you prevent the occurrence of cervical cancer
First, use a condom every time you have sex! Thus, you avoid exposure to HPV infection. Then the HPV vaccine is important. Prevention also includes routine gynecological examination and periodic Pap test, quitting smoking and taking care of your general health: Vitamins A, C, E and beta-carotene have been associated with a lower risk of cervical cancer.
How important is screening and how often should it be done
The Pap test (PAP) and the HPV test are the two recommended screening investigations that detect possible precancerous lesions before they turn into cancer – thus saving your life. These tests are simple, painless procedures that are performed at the gynecologist. Only one collection of cells is needed because they can also be tested for HPV, so there is no need for 2 checks.
Doctors recommend a Pap test every year starting at age 21. The HPV test identifies if you have been infected with the HPV virus. If you are over 30, gynecologists recommend this test together with the Pap test.
What do you need to know about the HPV vaccine?
Get vaccinated against HPV! In Romania, you can find 3 HPV vaccines (Gardasil, Gardasil 9 and Cervarix) that reduce the risk of precancerous changes in the cervix. Vaccines are effective for at least 8 years and are usually given from age 9 to 26.
Frequently asked questions
At what age can cervical cancer appear?
The risk of cervical cancer appears with the first sexual contact and persists throughout sexual life. An HPV infection must persist for a long time and be associated with a number of risk factors, but this is not the rule.
Can you still get pregnant if you have had cervical cancer?
If your uterus has not been removed and if your health after curing cervical cancer is good, then even if you had cervical cancer, you can become or become a mother again.






















